This is adapted from a presentation I gave at the hospital in November 2012, where my son, Connor, was born in December 2008 and graduated from his 120-day NICU stay. Details were taken from my personal account of our NICU experience and his NICU Timeline.

For over 2.5 years, Brian and I struggled with infertility. Finally, in June 2008, with some medical and divine intervention we were blessed and surprised with our first pregnancy!
Everything was going exceptionally well, nothing unusual, and we were anxiously anticipating the birth of our son in March 2009.
For reasons we will never understand, I began experiencing minor complications in early December 2008. It was a Saturday, so we headed to the hospital just to be safe. I spent over a week there, and was released home on bed rest, only to return a couple of days later in back labor.
That night, Connor was born by emergency C-section.
Rather than being the happiest day of my life, on this night, it turned into one of the scariest. I hadn’t quite hit the 3rd trimester – my son was over 13 weeks too early.
Miraculously, Connor emerged crying and breathing all on his own! Faster than we could blink, the NICU team prepped him and whisked him downstairs.
After his delivery, I wasn’t well. I had developed a blood infection, and for days I would experience raging fevers while the doctors tried to figure out a combination of antibiotics to cure the infection. The worst part about my recovery was the fact that I wasn’t allowed to see my baby for several days. Between the adjusting hormones, the feverish delirium, and the pain from recovering from surgery and bed rest, I was going out of my mind.
My husband spent most of his time with Connor in the NICU, and would bring me frequent updates. My mom had come into town and would stay in my room with me. The nurses printed out photos, and the neonatologists would consult with me on every decision in those early days. They all tried their hardest to keep me a part of the loop… but it just wasn’t the same as actually being there, in the NICU, with Connor. I was his mother – I needed to be with him.
Finally, on his 4th day of life, I was granted permission by the hospital’s infectious disease specialist to go see my son!
I can’t quite put into words what it was like to finally see him… amazing JOY with a heart so full I thought it would explode out of my chest.
The next day, when he was 5 days old, I was able to hold Connor for the very first time.
This baby we had struggled for, prayed for, and dreamed about was here… but way too soon. And, he had a long, hard road ahead of him.
When you land in the NICU, you’re told that it’s going to be a roller coaster ride – that there will be good days and bad days. Another preemie mom said, “They’ll say it’s a roller coaster ride, but they’ll leave out that you’re being dragged from the back by your ankles.” Your baby will likely make some amazingly good progress and the very next day will have serious, life-threatening setbacks while in the NICU. There’s really no better way to describe it.
Connor did really well, all things considered, for the first couple of weeks. He quickly moved from the CPAP to a cannula at room air for breathing. He developed brain bleeds on each side of his brain, a common occurrence in premature infants, which sometimes manifests later in life as a minor disability.
We celebrated Connor’s first Christmas with him in the NICU. It was bittersweet – we never imagined our son would have such a struggle ahead of him, but we were grateful he was alive.
Before dawn, on the day after Christmas, we received a call from the NICU saying they suspected Connor had developed NEC, or necrotizing enterocolitis, during the night. NEC involves infection and inflammation that causes destruction of the bowel. This dreaded and deadly disease occurs to about 10% of preemies weighing less than 3 pounds.
Connor had to be ventilated to ease the strain on his tiny, little body. His feeds were stopped, and the only comfort we could offer him was with our hands through the holes of his isolette – we could not hold him. For a very long week, we watched our little boy struggle. Day after day he required blood transfusions and his doctors were beginning to believe that sections of his bowel were actually dead from the disease.
On New Year’s Eve, Connor was wheeled into surgery where they removed 20cm of his intestines, roughly one-third, and he was given an ostomy. He weighed less than 3 pounds.
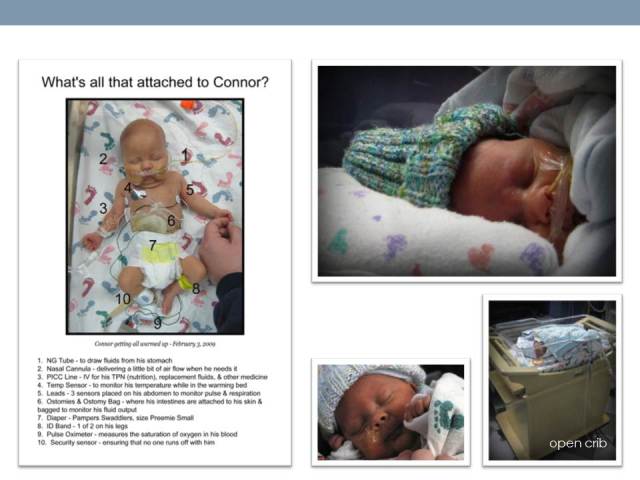
Connor continued to grow bigger and stronger. He was closely monitored regarding his brain bleeds, NEC, and ROP. He was able to better regulate his own body temp and graduated from an isolette to an open crib – which meant we would finally be able to hold him without the assistance of a nurse. His brain bleeds improved, but his ROP worsened to the point of requiring surgery. His second surgery was scheduled, to reattach his intestines, and then cancelled when he developed yet another infection. Up and down, up and down… like a roller coaster.
At 2 months old, his second surgery, to repair his intestines finally happened, and a week later a third, laser eye surgery to repair ROP damage.
Connor continued to grow, came off the ventilator again, his ROP began regressing.
When your premature baby is born, you’re told the best guess for discharge is around the baby’s original due date. For Connor this was around mid-March, when he would turn 3 months old. Every baby is different, and Connor was no exception.
Around 3 months old, Connor’s still busy growing, trying to tolerate increased volumes in feedings, and occasionally requiring a cannula to help with breathing. He develops reflux at this point in time, which slows his progress yet again.
At 101 days old, Connor has a bad spell, stops breathing and turns blue. He has developed sepsis, a severe blood infection.
But then he miraculously recovered from that infection, and kept getting stronger… and pretty soon, when he was 110 days old, we were told by his neonatologists to plan to bring him home on Good Friday!
And wouldn’t you know it, the roller coaster ride was headed downhill again. The night before discharge, Connor lost 7 ounces and became severely dehydrated.
Finally, at 120 days our NICU stay would end… we were able to FINALLY bring our little boy home after a nearly 4-month hospital ordeal.
Life at home with our little one was pure bliss. He was about the size of a newborn and had much the same temperament and habits. We felt like seasoned parents given our 4-month ordeal. All we wanted to do was hibernate and nest with Connor.
But, there’s no rest for the weary. While we were fortunate to bring him home without oxygen or other monitors, we had a barrage of follow-up appointments to take Connor to, beginning that same week, 11 different specialists, and 8 different medications to administer all throughout the day.
For every condition Connor developed in the NICU, (and I haven’t even mentioned all of them) he had to follow-up with a specialist. Our calendar was crazy… between seeing doctors and getting frequent lab work and other tests done, there was hardly a minute to sit still.
Time passed and slowly, but surely, Connor recovered from many of his issues and began graduating some of his specialists.
As he got bigger, new issues cropped up, most notably a moderate to severe case of brachycephaly, where his skull was misshapen and flat. After 4 months in the NICU, and having to remain on his back due to abdominal surgeries, it was bound to happen. Connor wore 2 different DOC Bands, reshaping helmets, for 23 hours a day for 6 months.
Throughout all of the follow-ups, we kept holding our breath, waiting for the next shoe to drop. When preemies are still so young, you don’t know for some time, what the repercussions of their prematurity might be. Maybe he’ll just experience developmental delays, perhaps he’ll have to wear coke-bottle thick glasses, maybe he’ll be diagnosed with cerebral palsy, and perhaps he’ll struggle with learning disabilities. We didn’t know what the future would hold for Connor – but, we focused on keeping a positive attitude – we decided that if we could survive a 4-month NICU stay, we could handle anything.
To date, Connor has had copious appointments with the following medical professionals in regards to his complications and prematurity…
1. Pediatrician
2. Nephrologist
3. Pediatric Dentist
4. Physical Therapist
5. Neurologist
6. Ophthalmologist
7. Speech Pathologist
8. Early Intervention Evaluations & Therapists
9. Surgeon
10. NICU Follow-Up Clinic
11. DOC Band Clinic
12. Hematologist
13. Endocrinologist
14. Gastroenterologist
15. County Home Health Nurse
But slowly, they’ve become unnecessary as Connor has continued to grow, develop, and THRIVE.
The small size and fragility of preemies is sometimes difficult for those outside the NICU experience to understand. To track Connor’s growth and to get a sense of perspective we began taking his picture with this stuffed monkey. We wanted to be able to visually compare just how far he had come from month to month for his first year.
NICU parents must learn early on to advocate for their children, to be their voices, and use their intuition, sometimes against the advice and opinions they’ve been given. No one knows their child better than the parent. Being your child’s advocate continues long after the NICU stay is over.
Being a NICU parent is very isolating. Physically isolating, because often, in order to protect their medically fragile children, families will sequester themselves at home while they’re very young, particularly during flu season, to avoid germs. Often, friends and family are even kept away, all to protect these little ones. Special efforts are made to avoid re-hospitalization.
It’s emotionally isolating, because it’s rare to know another parent who has been through what they’re going through. Your hopes and dreams can be dashed when you land in the NICU. I’ll always mourn that I never have the birth experience I dreamed about. I’ll never be able to make up for those days I was unable to comfort and hold him the way a baby needs. I’ll never get over the anguish I felt those 120 long days in the NICU. I’ll never reconcile my sorrow in leaving him behind night after night and not taking him home with me. I’ll never be able to forget the fear and terror I felt while watching him teeter so close to death. These are emotional scars I’ve had to grieve and work through. Studies now show that parents can develop PTSD after a traumatic childbirth experience.
This is why I co-founded a support group with a fellow NICU mom in 2011 – to help NICU parents know they’re not alone, and that they will make it through this difficult experience. We try to offer hope and encouragement to these families, who like us, have been through so much. We’ve held local Chicagoland events for families to get to know each other, and we manage an online support forum with over 10,000 followers as of August 2013.
Connor’s story is a success story. He is nothing short of a miracle. He is just a month from turning 4 years old, and aside from his small size and slight gross motor delays, you’d never know he was born 13 weeks premature. He began mainstream preschool in September and loves it. He’s smart as a whip, likely has a photographic memory, and is reading now. He does not have cerebral palsy, has vision better than most children his age, and eats and digests food like a champ, despite having 1/3 less intestines. While Connor had a horrific NICU stay compared to many, the absence of lingering “side effects” is nothing short of a miracle. We feel incredibly fortunate and lucky to have the outcome we did with him, given all that he went through… we do not take that for granted. Not every NICU story turns out the way ours has.
We credit and thank the amazing doctors, nurses, and support staff of the Rush-Copley NICU for all that they did for him and us. His outcome is also a reflection of your passion and hard work. We will always consider you part of our family. THANK YOU.